
Paying it forward: Why we need YOU to give blood - Part 6
In this six-part series, Dr. Jeannie Callum, a hospital-based transfusion specialist, shares her real-life experience witnessing the impact of blood donation on patient lives. She provides some fascinating insight into blood transfusion, past and present, and emphasizes the need for male donors and why some donors may be safer for patients. Read the complete series here.
- Part 1: A miraculous gift, ready and waiting
- Part 2: Not your average bank
- Part 3: Blood type hype
- Part 4: Beyond matching ABO and Rh: Rare blood challenges and international cooperation
- Part 5: All blood is not the same
- Part 6: My own donation journey...
Donating blood is a really minor procedure that takes about an hour. I have done it 28 times, which is actually not very many. One of the pharmacists at my hospital has donated over 100 times. I have donated whole blood, platelets, bone marrow, and stem cells — through apheresis. When it became understood that women were harming recipients from transfusion-related acute lung injury, I no longer could donate platelets. But I can still donate red cells.
In 2010, I received a call from the Canadian Blood Services’ bone marrow registry program “One Match” to tell me I had matched to someone and could I come back and have more definitive testing to confirm if I was the best donor for the patient. I went immediately to have the blood drawn, because the need for stem cell transplants are often urgent. I did not hear back for a few weeks. I was 41 years old at the time; one year above the usual “age” cut off. Typically, they want young stem cells before they are damaged through the process of aging. On the 23rd of December, I received a voice message at work asking me to call back. I was shaking. Partly excited that I might have been chosen and partly worried they were going to tell me I had failed to meet the cut (too old, the same female problem as mentioned above). But it was a yes and they wanted me to donate bone marrow.
Global differences in disease prevalence and HLA evolution help to explain why it’s easier to find an HLA match within your own ethnic group – and why it’s so important for people of all ethnic backgrounds to be adequately represented in the stem cell registry and cord blood banks.
Of course, I said yes. But then immediately called one of the transplant physicians to make sure bone marrow was medically necessary. It is only a 30-minute minor operation but you need a general anesthetic. It turned out it was necessary — for some bone marrow diseases patient outcomes are better with a bone marrow donation. The bone marrow harvest was completely uneventful. They took the equivalent of four units of blood or one litre of bone marrow fluid. My procedure was at 8 a.m. and by 10 a.m. I was in the hospital coffee line-up with my IV pole at Princess Margaret Hospital, the largest cancer centre in Toronto. By 4 p.m., I was home. Three days later I was back to work. A few weeks later they called me to say they didn’t get enough stem cells from the marrow and they needed more; the patient weighed more than me — likely a male recipient.
In a few weeks, with my bone marrow revved up with blood hormones, I donated stem cells through a special process called apheresis (it’s where you get hooked up to a machine that filters the white cells out of your blood). Shortly after the procedure, one of my pathology colleagues paged me to tell me he was looking at my blood film and he was worried I had leukemia. I laughed and reassured him it was just the hormones for the stem cell collection — my white count had risen from 4 to over 100 and that had sent him into a panic.
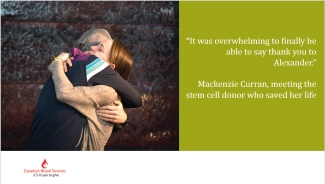
I was notified when my recipient received his transplant (I cried of course). I was sent a lovely letter from a family member, perhaps the grateful wife or mother, thanking me for donating. It was a cross border arrangement from Canada to the US. It is fascinating to think that my stem cells are somewhere in the US, hopefully nicely settled in their new environment.
Every time I donate blood I wonder where the unit goes. Units of red blood cells get released to a hospital about 7 to 14 days after collection, and typically get transfused within days of arriving at the hospital. There needs to be sufficient stocks to handle emergencies and the natural ups and downs of transfusion needs across the country.Did the unit go to a young girl recovering from chemotherapy for leukemia? A little boy born with a heart defect who needed surgery within days of birth? To someone in an industrial accident? Or someone needing cardiac surgery or an organ transplant? A patient with bone marrow failure waiting for a stem cell transplant? A child with sickle cell anemia that needs blood once to twice a month? Or a new little human that came months too soon who needs my blood to nourish them for their first 42 days of life?
Thank you!
If you donated blood in this past year, thank you! Words cannot express how much you do for our patients. After 17 years of practicing transfusion medicine, I am still surprised at how miraculous the whole thing is. You are asked to come in to donate blood. You show up, no questions asked about what is done with the blood. And each and every time you save a life. And you come back year after year. You are a hero.

There are some of you who are completely healthy, and eligible, and didn’t donate last year. Listen to what I have to say: donating blood is very easy. It takes about an hour or so. If you are worried about the needle, don’t look when they put it in or take it out — it doesn’t really hurt going in and you can’t feel it coming out. If you are worried about fainting, you can prevent that by drinking lots of fluids the day before and for three days after. Adding more salt the day before also helps — reward yourself with a bag of salted chips. If you think you don’t have time, please think twice. Everyone can spare at least one hour or two per year to save a life.
□ All blood types are needed but a particular need remains for O negative blood because it is the only type compatible with all other blood types.
□ The demand for blood never stops; cancer patients, accident victims, and people with blood disorders rely on blood transfusions every day.
□ New donors are critical to meeting Canada’s future blood needs.
Someday you may be on the receiving end of a blood transfusion, or someone you love will be. About half of us will need a transfusion someday, and usually it’s more than just one unit. Once you get sick, you will likely never be able to be a blood donor. So now's your chance.
You need to pay it forward — it’s the only way this works. If you are a strapping lad in the prime of your life and you have never donated before and you meet the criteria to donate (i.e. no tattoos in the last six months), go to the mirror and have a conversation with yourself. Then go to blood.ca to make an appointment to donate. Please don’t forget to show up, I am — we are — counting on you.
This post is the last in the six-part series "Paying it Forward: Why we need YOU to give blood". We are sincerely grateful to Dr. Callum for allowing us to publish this series on RED.
Dr. Jeannie Callum, Staff Hematologist and Director of Transfusion Medicine and Tissue Banks, Sunnybrook Health Sciences Centre, and Associate Professor, Department of Laboratory Medicine and Pathobiology, University of Toronto.
Canadian Blood Services – Driving world-class innovation
Through discovery, development and applied research, Canadian Blood Services drives world-class innovation in blood transfusion, cellular therapy and transplantation—bringing clarity and insight to an increasingly complex healthcare future. Our dedicated research team and extended network of partners engage in exploratory and applied research to create new knowledge, inform and enhance best practices, contribute to the development of new services and technologies, and build capacity through training and collaboration. Find out more about our research impact.
The opinions reflected in this post are those of the author and do not necessarily reflect the opinions of Canadian Blood Services nor do they reflect the views of Health Canada or any other funding agency.
Related blog posts
In this six-part series, Dr. Jeannie Callum, a hospital-based transfusion specialist, shares her real-life experience witnessing the impact of blood donation on patient lives. She provides some fascinating insight into blood transfusion, past and present, and emphasizes the need for male donors and why some donors may be safer for patients. Read the complete series here.
In this six-part series, Dr. Jeannie Callum, a hospital-based transfusion specialist, shares her real-life experience witnessing the impact of blood donation on patient lives. She provides some fascinating insight into blood transfusion, past and present, and emphasizes the need for male donors and why some donors may be safer for patients. Read the complete series here.

