Sickle cell disease and blood donation
Sickle cell disease is the most common inherited condition in Canada. Over 6,000 people across the country are currently living with sickle cell disease — and that number is continuing to grow.
Donors of blood, plasma, platelets and stem cells all play a vital role in supporting the treatment of people with sickle cell disease. Many with this condition, including children, depend on donated blood and blood components to treat their symptoms, or even to help save their lives.

Blood components from donors of a similar ethnic background or ancestry lead to the best outcomes
In Canada, insufficient ethnic diversity in our donor base is one of the biggest challenges we face in supporting people living with sickle cell disease.
Those who receive frequent blood transfusions — and those with rare blood types — need blood with the closest match possible. Since blood types are inherited, this means that people living with sickle cell disease often rely on blood from donors of similar ancestry.
Did you know?
- In Canada, blood transfusion is one of the few treatments available to people living with sickle cell disease.
- Blood transfusions can be used to treat various health problems caused by sickle cell disease. Sometimes, only a single transfusion is needed. In other situations, people need regular red blood cell exchanges (where the patients’ sickled red blood cells are removed and replaced with a donor’s red blood cells). Such exchanges may occur every four to six weeks, for life.
- The most well-known blood group is ABO (which includes blood types A, B, AB and O), but in fact there are more than 33 blood groups. A person’s type within each group determines the combination of more than 300 markers on that person’s red blood cells, all of which are inherited from their ancestors.
- Sickle cell disease is more frequent among those whose ancestors are from Africa, the Caribbean, Central and South America, the Middle East and South Asia. People with similar ethnic backgrounds or ancestry to those living with sickle cell disease have the greatest potential to help as blood donors.
- Donors of all ages and ethnic backgrounds are needed to support patients, including those with sickle cell disease, who will need transfusions throughout their lives. The earlier you begin donating, the more lives you can help save. Young people can begin donating blood and plasma as early as age 17.
Living with sickle cell disease
Ulysse Guerrier received a sickle cell disease diagnosis when he was just two years old.
In sickle cell disease, the body cannot produce enough functional red blood cells, which means that those affected may require regular red blood cell exchange treatments.
Ulysse currently receives seven to twelve units of blood every month. Over the course of his life so far, he’s received more than 10,000 blood transfusions.
As a person living with sickle cell disease, Ulysse encourages all eligible people in Canada to donate blood, especially those from African, Caribbean and Black communities.
[Sickle cell] is not a Black person’s disease, it’s a red blood cell disorder. As long as you have blood going through your veins, there is a possibility that you could carry the gene…It’s very important to have a bigger pool of diverse donors. There are a lot of people like me who need blood.
– Ulysse Guerrier, blood recipient living with sickle cell disease

Three easy ways you can help people with sickle cell disease
- Schedule an appointment to donate blood or plasma. We need the donor pool to be as big and diverse as possible. If you’re 17 or older, find out if you’re eligible to donate today (and encourage your friends and family to do the same).
- Join the Sickle Cell Disease Association of Canada’s Partners for Life team, a national movement to support people living with sickle cell disease.
- If you’re already a blood or plasma donor, remember to donate regularly. For many people living with sickle cell disease and other conditions, the need for blood is ongoing.
About sickle cell disease
What is sickle cell disease?
Sickle cell disease is a debilitating condition that affects approximately 6,000 people across Canada. It is not contagious. The disease is caused by an inherited mutation in hemoglobin, a protein in red blood cells that carries oxygen to the body’s organs and tissues and transports carbon dioxide back to the lungs.
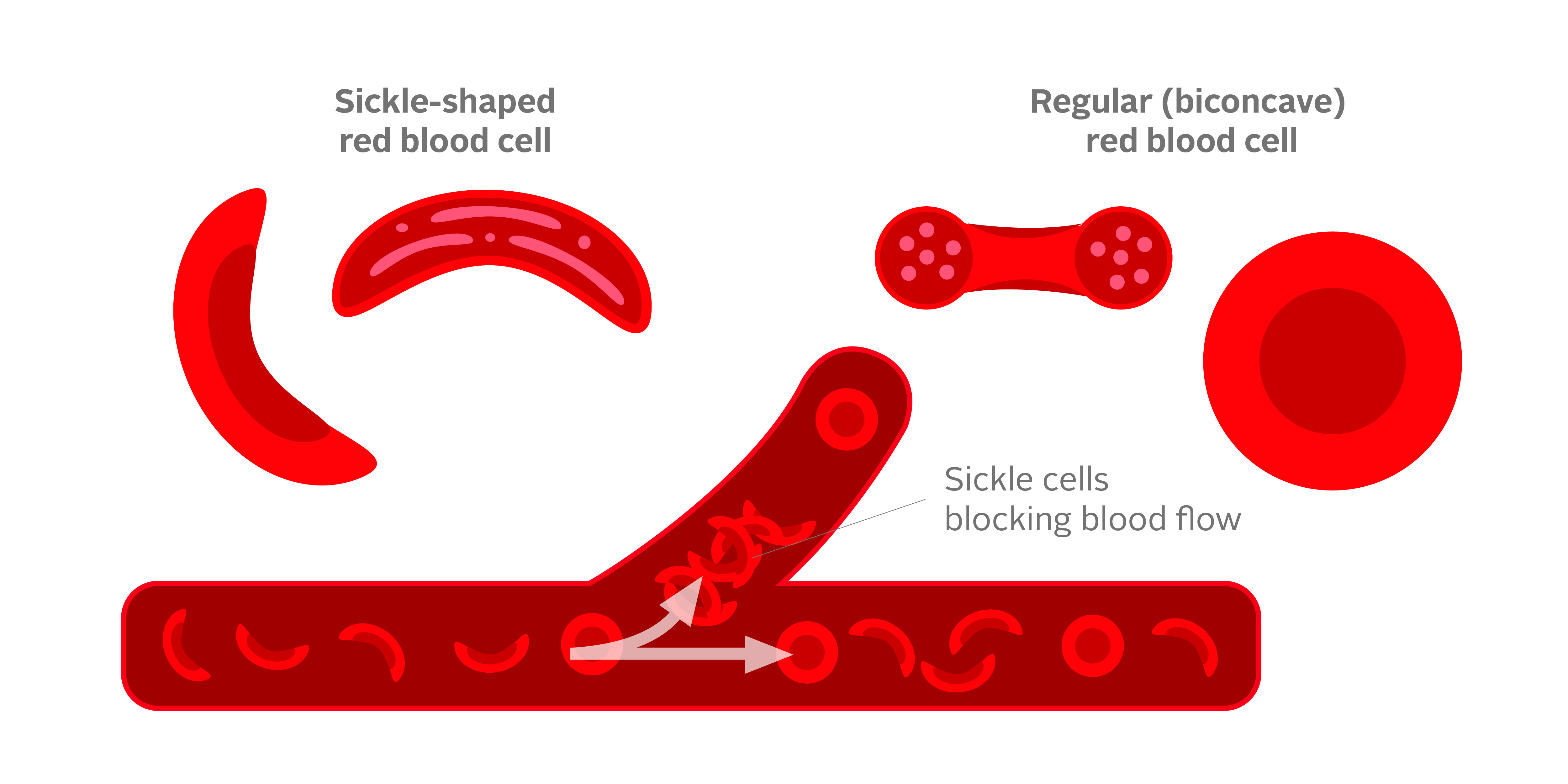
How are sickled cells different from non-sickled cells?
Unlike regular red blood cells that are soft, round and can squeeze through tiny blood vessels, sickled cells are rigid, with a sickle-like shape. This means they are unable to freely move through smaller blood vessels, which can sometimes cause blockages.
What are the complications of sickle cell disease?
People with sickle cell disease may experience serious complications such as severe pain episodes, breathing problems, stroke, and even multiple organ failures. Complications are often treated with antibiotics, pain management, intravenous fluids, blood transfusion and surgery. In rare situations, some with extremely severe disease and a family member who is a match may be considered for a stem cell transplant. For most, however, there is no cure.
Meeting the need for matched blood
Regular blood transfusions
A close blood type match is essential for people living with sickle cell disease who need regular blood transfusions. That’s partly because of the increased chance of side effects that comes with the large number of transfusions these people may require over their lifetime.
Importance of matching antigens
Every person’s red blood cells are covered with markers called antigens. These markers determine each person’s extended blood type (beyond their ABO group). When a patient receives a blood transfusion from a donor with a different combination of antigens from their own, their body may produce antibodies that attack the unfamiliar antigens. To prevent such attacks, it’s crucial to find donors whose red blood cell antigens match those of the recipient. And because blood type is inherited, a closer match may be found among donors with similar ancestry.
Canadian Blood Services is committed to improving transfusion outcomes for people living with sickle cell disease.
Current initiatives include:
- Proactively managing our red blood cell inventory to selectively identify blood units and ensure sufficient monthly supply for people with sickle cell disease who need regular transfusions.
- Expanding the number of donors who undergo testing for blood groups and compatibility, as well as the blood group antigens for which they’re tested, to better support patients through our rare blood program.
- Building and strengthening partnerships with community organizations across Canada to enhance donor recruitment and retention.
- Assessing barriers to donation that may affect the supply of blood for patients from certain communities.
Sickle cell FAQs
How can I become a blood donor?
If you’re thinking about donating for the first time, here are a few simple steps you can take:
- Find out if you’re eligible. Take the quiz and learn more about the eligibility criteria.
- Find a donor centre near you.
- Book an appointment. Booking in advance helps our clinic run smoothly and also helps us ensure your first donation experience is a good one.
- Learn more about the blood donation process.
Still have questions? Sign up for more information by email or call to speak with one of our trained healthcare professionals at 1 888 2 DONATE (1-888-236-6283).
Why do people with sickle cell disease need donors of the same or similar ethnic ancestry?
Those living with sickle cell disease bring the importance of an ethnically diverse blood supply sharply into focus.
People with sickle cell disease may need regular red blood cell transfusions, and the most compatible blood may come from donors of similar ethnic ancestry. Unlike other transfusion recipients, people living with sickle cell disease have a greater likelihood of experiencing side effects from transfusions. That is partly because of the high number of transfusions they receive over the course of their lives, and partly because of the disease itself. Providing the most compatible blood helps minimize these side effects.
With each transfusion, recipients are exposed to donors’ red blood cell markers, called antigens. If antigens are mismatched, the recipient’s immune system can form antibodies to the antigens that differ from their own. Compared with others who receive red blood cell transfusions, people with sickle cell disease are 10 times more likely to develop antibodies to donor antigens. Once these antibodies form, finding compatible blood for future transfusions becomes more difficult.
Because blood antigens are inherited, antigen-matched blood is more likely to be found in someone whose ancestry resembles that of the recipient.
Sickle cell disease is more frequent among those whose ancestors are from sub-Saharan Africa; Spanish-speaking regions in the Western Hemisphere (South America, the Caribbean, and Central America); Saudi Arabia; India; and Mediterranean countries such as Turkey, Greece and Italy. People whose ancestors are also from these regions have the greatest potential to help people with sickle cell disease, as donors.
How does Canadian Blood Services find the most compatible donors for people with sickle cell disease?
Canadian Blood Services has processes in place to identify matched blood from our large inventory of red blood cell units. These processes include, but are not limited to:
- ongoing recruitment and retention of a large and increasingly diverse donor base
- partnerships with community organizations to help support the recruitment of donors from a wide range of ethnic backgrounds
- testing donors for the antigens commonly found in patients with sickle cell disease
- our rare blood program, which consists of a team of health care professionals who support hospitals by providing individualized patient assessments and by finding optimally matched blood units within our inventory
Can I donate blood if I have sickle cell trait?
Yes! People with sickle cell trait are eligible — and encouraged — to donate blood. If you have never donated blood, plasma or platelets before, we encourage you to call 1 800 2 DONATE (1-888-236-6283) to discuss your eligibility.
Is Canadian Blood Services currently meeting the needs of people with sickle cell disease who require blood components?
Yes. Canadian Blood Services continues to meet the transfusion needs of people with sickle cell disease through our existing donor base, and by importing products from other blood operators around the world. In 2022, we distributed more than 15,000 units of red blood cells for transfusion to people in Canada living with sickle cell disease and other inherited disorders such as thalassemia.
However, the increasing population of people living with sickle cell disease, along with the growing need for more precise matching of blood groups, are driving the need for more — and even more compatible — donors.
How much iron do I need to donate blood, platelets and/or plasma?
At every donation, we check your hemoglobin level using a fingerprick test. Hemoglobin contains iron, and low hemoglobin levels in blood donors are often due to inadequate iron. For whole blood, platelets and some plasma donation, the minimum hemoglobin level required is different based on donors’ gender at registration. Hemoglobin level requirement is 125g/L for donors registered as female and 130g/L for donors registered as male.
Canadian Blood Services is currently taking steps to help donors manage their iron stores, by selectively testing blood donors’ ferritin levels. The intent is to enhance donor experience by proactively helping to prevent low iron in donors.
Learn more about iron and blood donation
Learn more about ferritin testing
Can people who have travelled to malaria-endemic regions donate whole blood, plasma, or platelets?
If you have travelled to a malaria-endemic region where preventative medications are recommended, your waiting period to donate whole blood or platelets will depend on the length of your stay in certain regions. This is because the chance of having a new or previously unrecognized infection diminish over time.
- If your stay was less than one day, you may be able to donate depending on where you were.
- If your stay was less than six (6) months, you will need to wait three (3) months from the date you left a malaria-endemic region.
- If your stay was six (6) months or more, you will need to wait three (3) years.
If your visit lasted less than 24 hours, please call us at 1 888 2 DONATE (1 888 236-6283) to discuss your eligibility.
Learn more travel and/or living internationally and blood donation.
Learn more about malaria and blood donation.
Can people who have had malaria donate whole blood, plasma, or platelets?
Unfortunately, at this time, there is no suitable, Health Canada-approved screening test available that can adequately screen blood donors for malaria. In the absence of an available test in Canada, we rely on thorough donor eligibility assessments based on possible exposure to the illness.
This means that if you have had malaria — even if you have fully recovered — you are not eligible to donate whole blood or platelets.
However, you may be able to donate plasma used to manufacture lifesaving medications. You may also be able to donate stem cells, organs and/or tissues.
How is sickle cell trait different from sickle cell disease?
Sickle cell trait is not the same as sickle cell disease. Sickle cell disease occurs when a person inherits two sickle cell mutations affecting the hemoglobin, one from each biological parent. People who inherit just one mutation (from one parent) are called “carriers” and are said to have sickle cell trait. Individuals with sickle cell trait do not have the disease and do not experience any symptoms.
In contrast, in people with sickle cell disease, the red blood cells can become elongated and rigid, often described as being crescent- or sickle-shaped. When this happens, the red blood cells last less than the usual 120 days in circulation, and they also tend to get stuck when moving through small blood vessels throughout the body. As a result, a person with sickle cell disease has a shortage of the softer and rounder red blood cells. People living with sickle cell disease may experience pain, fatigue, shortness of breath and dizziness.
Sickle cell disease is classified further according to the particular hemoglobin mutations that are present. This gives rise to the various subtypes that you may hear about, such as hemoglobin SS disease, hemoglobin SC disease and hemoglobin S beta-thalassemia.
What’s the difference between thalassemia and sickle cell disease?
Thalassemia and sickle cell disease are both genetic disorders that affect the hemoglobin in red blood cells, but they do so in different ways. A person who has thalassemia can’t make enough normal hemoglobin, so the quantity of hemoglobin is decreased. As a result, such patients have fewer red blood cells, and their red blood cells appear smaller than normal.
In sickle cell disease, many of the red blood cells are “sickled” into a crescent shape. Sickled cells can clog small blood vessels, preventing the delivery of oxygen around the body. This causes complications, such as pain, breathlessness, strokes and blood clots, and may even affect the functioning of the vital organs.
Sickle cell social media toolkit
This social media toolkit contains pre-built tiles containing information about sickle cell disease and the need for blood donors from ethnically diverse communities. We encourage you to share these tiles on your social media accounts and with your networks, to help inspire more people to join Canada’s Lifeline.




